Understanding the Causes of SpO2 Cable Signal Interference
Common Sources of Interference in Clinical Environments
Hospitals today are full of all sorts of electromagnetic interference (EMI) that messes with how well SpO2 cables work. Think about fluorescent lights buzzing overhead, those big MRI machines humming away, and even those wireless infusion pumps sending signals around the place. These devices operate in the 2.4 to 5 GHz range, right where pulse oximeters pick up their readings too. According to a recent study from clinical engineers back in 2023, almost two thirds of those annoying false low oxygen alerts actually come from either electrosurgical equipment during procedures or those modern Bluetooth patient call buttons scattered throughout wards. And don't forget about those old electrical outlets that weren't properly shielded when installed years ago, plus mobile workstations that somehow never got grounded properly. All this creates signal problems for medical staff trying to monitor patients accurately anywhere within about 1.5 meters of these trouble spots.
How Electromagnetic Interference Disrupts SpO2 Signal Accuracy
Electromagnetic interference messes up the signals from SpO2 sensors because it gets in the way of how those red and infrared lights measure blood flow. We saw this happen during some ventilator sync checks where cables without proper shielding near those 50 Hz AC fields from hospital monitors had about 22% more signal problems compared to their shielded counterparts. What makes this really concerning is that these disturbances look just like actual blood pulses, which means doctors might see fake heart rates or think patients have dangerously low oxygen levels when they actually don't. This kind of error could lead to unnecessary treatments or missed warnings about real health issues.
Cross-Talk and Interference Coupling in High-Density Ward Setups
A 2024 study on critical care found that in intensive care units where beds are spaced six feet apart or closer together, there's about a 40 percent increase in cross interference incidents. When SpO2 cables run parallel between neighboring patient monitors, they create what's called capacitive coupling. This basically lets interference jump from one line to another, creating these annoying 10 to 300 millivolt echoes that can throw off readings. Things get even worse with those centralized monitoring towers because they often share power strips. The result? Harmonic resonances start happening which make waveforms look all messed up and hard to read accurately.
Impact of Patient Movement and Equipment Vibration on Readings
Ambulation or bed transfers introduce motion artifacts via cable microphonics—mechanical vibrations converted into electrical noise. Pneumatic compression sleeves produce 5–12 Hz vibrations, which overlap with normal pulse frequencies (0.5–3 Hz), potentially obscuring true bradycardia. Anti-microphonic cable jackets reduce these errors by 58% in ambulatory dialysis patients.
Rising Trends in Signal Noise Due to Multi-Device Overload
Hospitals are seeing a dramatic rise in wireless gadgets these days. The average count sits at around 14.7 devices per bed, which represents an impressive jump of over 200% compared to what we saw back in 2018. All this equipment creates serious radio frequency problems, leading to what experts call "spectral clashes." These clashes have an unexpected side effect - standard SpO2 monitoring cables are starting to act like antennas themselves. Recent studies from 2023 across 23 different hospitals show something alarming too. Noise levels in those crucial 500 to 600 MHz medical telemetry bands have climbed by about 11 decibels since before the pandemic hit. This makes it much harder for doctors to process signals properly when dealing with all the background interference from newer technologies like Wi-Fi 6E and 5G networks running alongside them.
Evaluating and Selecting Shielded SpO2 Cables for EMI-Heavy Wards
How Shielded Cables Reduce Noise in Multi-Parameter Monitoring Systems
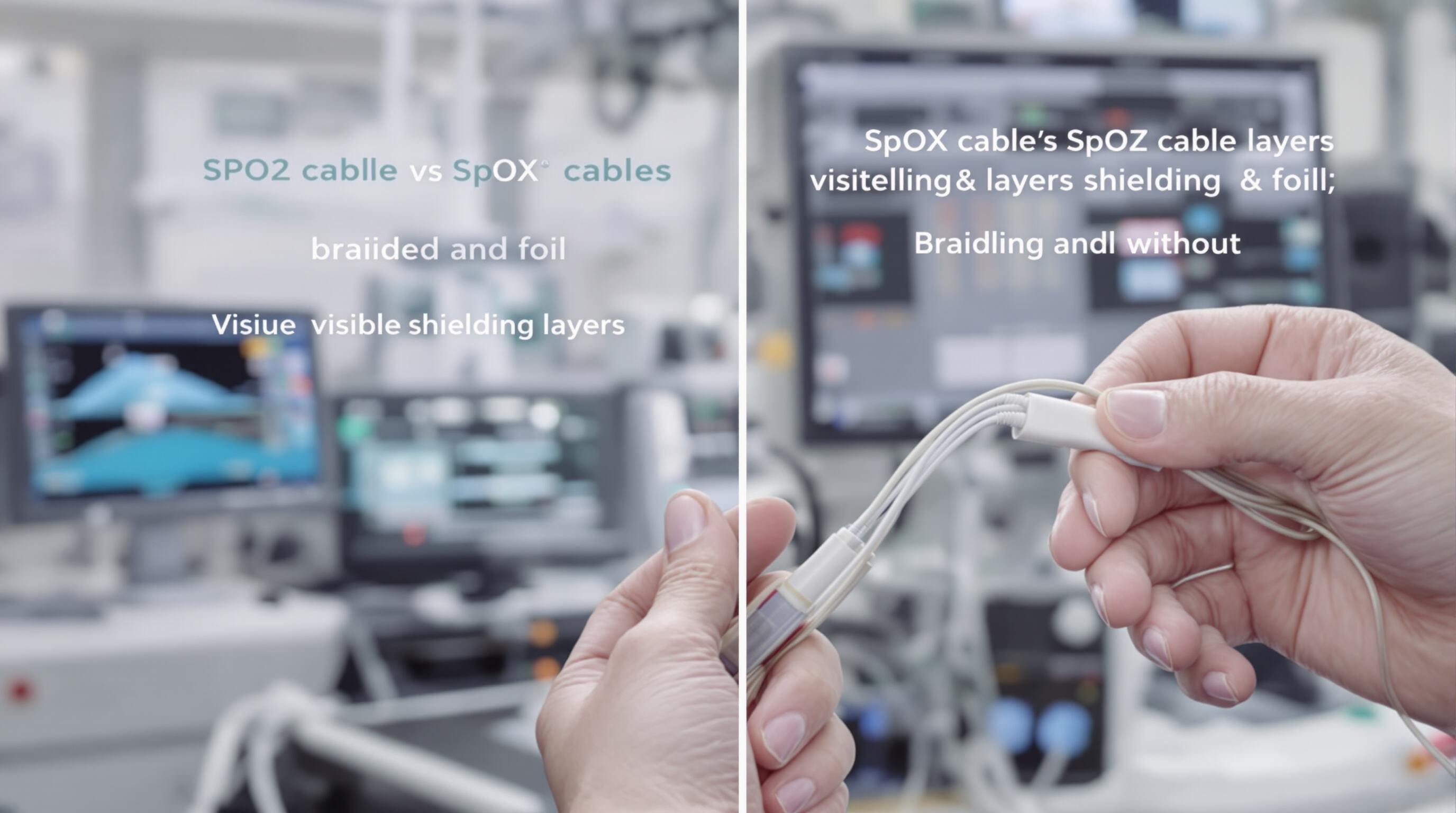
SpO2 cables with shielding have conductive materials like braided copper or aluminum foil built into them to block out electromagnetic interference. When working in areas with strong electromagnetic fields over 50 volts per meter according to IEEE standards from last year, shielded cables cut down on signal problems about 74 percent better than regular cables without shielding. The shielding makes all the difference in complex monitoring setups where things like heart rhythm readings and blood pressure checks get messed up if different signals interfere with each other across multiple devices.
Shielded vs. Unshielded SpO2 Cables: Performance in High-Interference Zones
| Factor | Shielded Cables | Unshielded Cables |
|---|---|---|
| Baseline SNR* | 28 dB | 14 dB |
| Post-Interference SNR | 24 dB (-14% loss) | 8 dB (-43% loss) |
| False Alerts/Day | 1.2 | 5.7 |
| *Signal-to-Noise Ratio in 20-device ICU simulation (2023 clinical trial) |
Shielded cables maintain 92% waveform integrity when defibrillators and infusion pumps operate simultaneously, compared to 58% for unshielded models.
Advancements in Shielding Materials and Design for SpO2 Cables
Recent innovations include:
- Hybrid shielding: Combines spiral-wrapped aluminum with nickel-coated polyester for full 360° EMI deflection
- Flex-core conductors: Reduce stiffness by 40% while maintaining over 85% shield coverage
- Dielectric gels: Fill microgaps between shielding layers, preventing interference coupling in vibrating environments
These advancements address the 63% rise in multi-device interference documented in modern ICUs (2024 Hospital Connectivity Report).
Ensuring Reliable SpO2 Cable Connections and System Integrity
Role of Auto-Locking Connectors in Maintaining Signal Stability
Auto-locking connectors minimize signal disruptions by reducing accidental disconnections by 83% compared to standard designs (Journal of Clinical Engineering, 2023), thanks to spring-loaded interfaces that ensure consistent electrical contact. Hospitals using auto-locking SpO2 systems report 67% fewer signal dropouts during patient transfers or equipment adjustments.
Effects of Frequent Plugging/Unplugging on SpO2 Cable Performance
Repeated connector cycling degrades gold-plated contacts, increasing electrical resistance by up to 40% after 5,000 insertions. This leads to intermittent signal loss and higher error rates in oxygen saturation readings. Cables subjected to more than 10 disconnections daily require replacement 50% sooner than those used in controlled settings.
Best Practices for Connector Handling and Cable Routing in Busy Wards
- Rotation Protocol: Rotate among 4–6 SpO2 cables weekly to distribute wear
-
Routing Standards:
Parameter Recommendation Minimum bend radius 5× cable diameter Proximity to EMI sources >12 inches from infusion pumps - Cleaning: Use alcohol-free wipes to avoid insulator degradation
Clinical trials show these practices reduce premature cable failures by 72% in ICUs with over 30 monitoring stations. Proper strain relief at connector junctions preserves internal shielding, ensuring sustained signal accuracy.
Implementing Clinical Protocols to Prevent and Manage Interference
Routine Maintenance of SpO2 Sensors and Cables to Avoid Degradation
Regular inspection and cleaning reduce oxidation and connector wear, which contribute to 22% of pulse oximetry signal degradation (Journal of Clinical Monitoring, 2023). Conduct monthly checks for frayed shielding or loose connectors, especially in high-use areas like ICUs. Use manufacturer-approved disinfectants to prevent residue buildup that could compromise insulation.
Standardized Protocols During Patient Transport and Shift Transitions
Implement checklists for cable management during bed transfers, where 63% of accidental disconnections occur. Require dual verification of SpO2 connections during nurse shift changes to ensure secure attachment. Designate “interference-sensitive zones” near MRI suites or wireless router clusters where cables must provide over 90 dB of attenuation.
Staff Training: Identifying and Responding to Interference Artifacts
Train clinicians to differentiate true hypoxemia from signal artifacts using waveform analysis. Simulation-based training reduces false alarms by 38% when staff recognize:
- Sudden waveform flattening without clinical correlation
- Persistent signal loss coinciding with equipment use
- Cyclical interference patterns aligned with nearby device frequencies
Emerging Trends: AI-Driven Interference Detection in Modern Monitoring Systems
Machine learning algorithms now detect anomalous SpO2 signals with 94% accuracy by analyzing:
- Local EMI source logs from facility databases
- Real-time electrical noise floor data
- Historical patient vital sign trends
Procurement Strategy: Assessing SpO2 Cable Quality and Shielding Efficacy
Prioritize cables that meet or exceed IEC 60601-1-2 standards for radiated immunity (minimum 10 V/m). Evaluate shielding effectiveness using key metrics:
| Metric | Clinical Relevance |
|---|---|
| Capacitance symmetry | Minimizes cross-talk in dense ward setups |
| Shield coverage | Blocks ≥85% of noise in the 900 MHz–2.4 GHz range |
| Flex cycle durability | Ensures integrity after 5,000 bending cycles |
FAQ
What causes interference in SpO2 cables?
Various sources like electromagnetic interference from medical equipment such as MRI machines, electrosurgical equipment, and Bluetooth devices can cause signal interference in SpO2 cables.
How does EMI affect SpO2 signal accuracy?
EMI can cause signal problems that mimic real blood pulses, leading to inaccurate readings of heart rates and oxygen levels.
Why are shielded SpO2 cables recommended?
Shielded cables reduce signal interference by blocking electromagnetic fields, thereby maintaining better signal integrity.
How often should SpO2 cables be maintained?
Regular inspection and cleaning should be performed monthly to reduce oxidation, wear, and potential signal degradation.
What are some best practices for reducing SpO2 cable interference?
Implementing rotation protocols, following cable routing standards, and training staff to recognize interference artifacts are effective practices.
Table of Contents
-
Understanding the Causes of SpO2 Cable Signal Interference
- Common Sources of Interference in Clinical Environments
- How Electromagnetic Interference Disrupts SpO2 Signal Accuracy
- Cross-Talk and Interference Coupling in High-Density Ward Setups
- Impact of Patient Movement and Equipment Vibration on Readings
- Rising Trends in Signal Noise Due to Multi-Device Overload
- Evaluating and Selecting Shielded SpO2 Cables for EMI-Heavy Wards
- Ensuring Reliable SpO2 Cable Connections and System Integrity
-
Implementing Clinical Protocols to Prevent and Manage Interference
- Routine Maintenance of SpO2 Sensors and Cables to Avoid Degradation
- Standardized Protocols During Patient Transport and Shift Transitions
- Staff Training: Identifying and Responding to Interference Artifacts
- Emerging Trends: AI-Driven Interference Detection in Modern Monitoring Systems
- Procurement Strategy: Assessing SpO2 Cable Quality and Shielding Efficacy
- FAQ


