Understanding Pressure Infusion Bags and Associated Clinical Risks

What Are Pressure Infusion Bags and How Do They Function?
Pressure infusion bags serve as medical tools meant to speed up how fast fluids get into patients by putting extra pressure on regular IV fluid containers. These devices basically wrap around standard IV bags with an inflatable part inside. Medical staff then pump air into this bladder area, usually reaching pressures between 200 and 300 mmHg either manually or through automatic systems. What happens next is pretty straightforward physics: the pressure difference pushes the fluids through the tubes much quicker than just relying on gravity alone. Although these bags work great when time matters most during emergency situations, don't let their simple design fool anyone. Behind those seemingly uncomplicated mechanisms lies quite a bit of complexity in actual practice. Studies indicate something interesting here too - almost all nurses have to refill these bags halfway through procedures simply to keep the fluids flowing at the right speed according to what doctors need.
Common Risks of Air Embolism and Overpressure in Clinical Use
Improper calibration exposes patients to two critical hazards:
- Air embolism: Residual air in pressurized systems can enter the vasculature, with as little as 100–300 mL proving fatal. A national survey found that 79% of emergency clinicians express concern about this risk during pressure bag use.
- Tissue extravasation: Excessive pressure (>300 mmHg) may rupture veins, especially in elderly or pediatric patients. Although modern systems include pressure relief valves, a 2021 analysis revealed 34% of units lack real-time pressure monitoring, increasing vulnerability to overpressure events.
Flow Rate Variability and Its Impact on Patient Therapy
Maintaining consistent flow really comes down to keeping up the pressure, which gets harder as the amount of fluid in the bag goes down. Research indicates that when they drain about 600 mL out of a standard 1 liter bag without adjusting the pressure, the flow rate plummets around 42%. This kind of fluctuation creates problems for emergency treatment protocols that depend on delivering exact amounts of fluids each minute. Clinicians have started implementing several strategies to deal with this issue including checking pressures every hour, training staff when to reinflate bags properly, and using automated systems whenever possible. What many don't realize is how big the difference actually is between what flows at first (usually somewhere between 300 and 500 mL per minute) versus later stages when it drops below 150 mL per minute. This discrepancy continues to disrupt treatment effectiveness despite all these efforts.
The Science of Pressure Calibration in Infusion Systems
Precise pressure calibration ensures patient safety while maintaining therapeutic flow rates. Modern pressure infusion bags must meet ISO 60601-2-34 standards, which require calibration tolerances within ±2%; deviations increase risks of vein damage from overpressure or underperfusion (Ponemon Institute 2023).
Principles of Pressure Calibration in Medical Devices
Calibration involves comparing device readings against traceable reference instruments under controlled conditions. For pressure infusion systems, hydraulic or pneumatic test pumps simulate physiological pressure ranges (200–300 mmHg). Discrepancies are corrected via proprietary algorithms to align outputs with international safety benchmarks.
Key Factors Affecting Calibration Accuracy and Usability
Three variables most impact calibration reliability:
- Environmental conditions: Temperature fluctuations >5°C alter fluid viscosity and bladder elasticity
- Operator training: Improper inflation techniques account for 34% of calibration errors (Journal of Clinical Engineering 2022)
- Device wear: Membrane fatigue in reusable systems reduces pressure consistency by 0.8% per 100 cycles
PSI vs. mmHg: Measuring and Interpreting Pressure Thresholds
PSI or pounds per square inch gets plenty of use in industry settings, but when it comes to actual medical work, doctors rely on mmHg (millimeters of mercury) because this unit actually matches how blood vessels behave under pressure. Getting these units right matters a lot since there's about 51.7 mmHg in each pound of pressure. Most hospitals don't worry about converting manually anymore thanks to smart infusion pumps that take care of math automatically behind the scenes. According to recent guidance from the American Heart Association, proper mmHg calibration remains essential across all vascular treatments to avoid any mixups in medication amounts. After all, nobody wants errors creeping into patient care just because someone missed a decimal point somewhere along the line.
Step-by-Step Calibration Best Practices for Pressure Infusion Bags
Pre-Use Inspection and Initial Inflation Techniques
Begin each calibration cycle with a thorough inspection for visible damage, leaks, or worn connectors. Ensure the cuff bladder inflates evenly and maintains structural integrity during preliminary tests. A 2023 clinical safety audit found that 18% of calibration errors stem from undetected material degradation in aging devices.
Applying Standardized Calibration Procedures for Consistent Pressure Delivery
Follow AAMI/ANSI guidelines for medical device calibration, adjusting settings to account for ambient temperature and fluid viscosity. Use a calibrated reference gauge to cross-validate output during adjustment to the 200–300 mmHg target range.
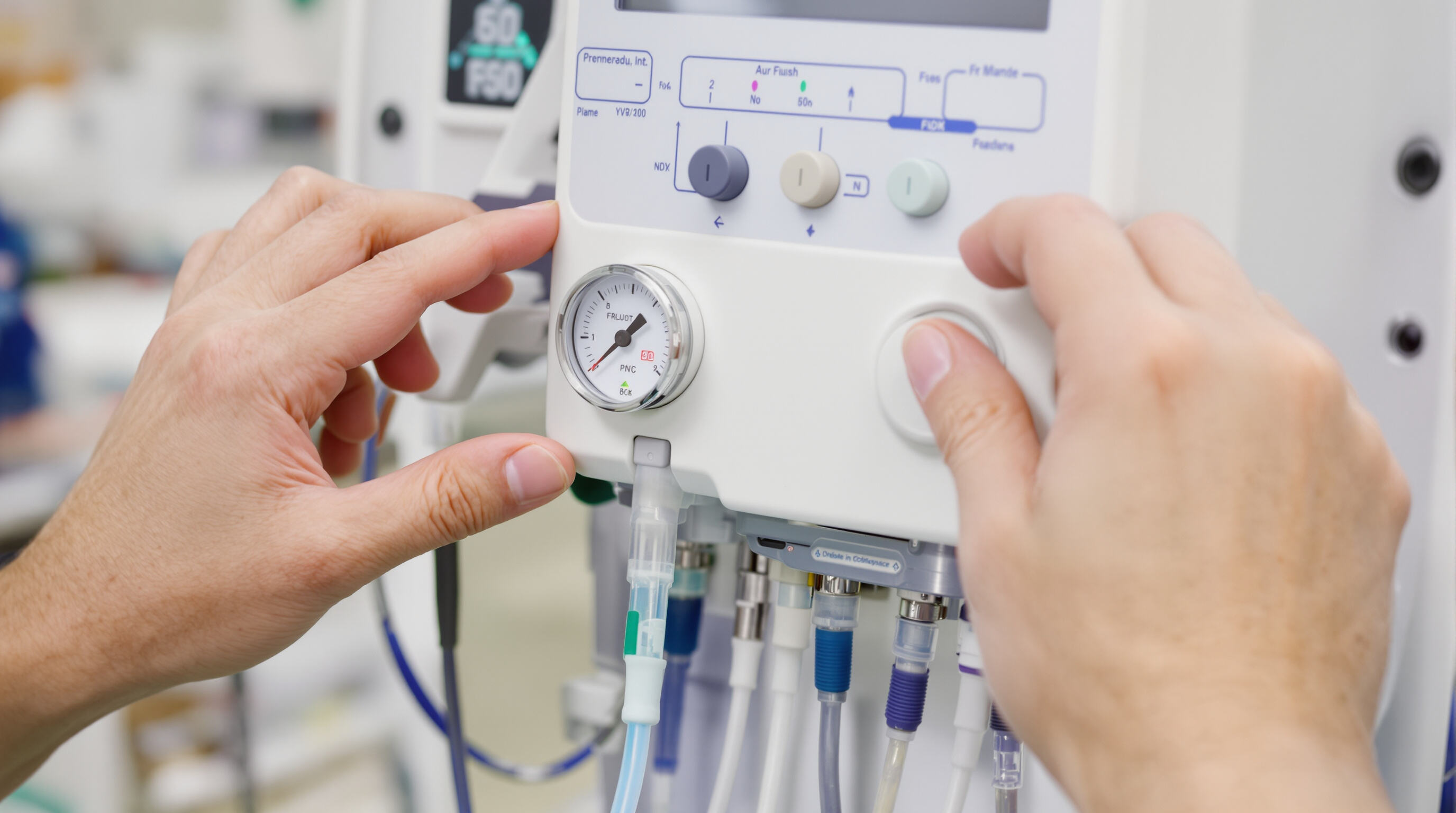
Using Pressure Gauges to Achieve and Verify 200–300 mmHg Target Range
Select gauges with ±1% accuracy to minimize drift during rapid infusion. Confirm stability by monitoring readings for at least 90 seconds post-inflation; pressure drops exceeding 10% indicate seal failure or air leakage.
Documenting Calibration Settings and Re-Inflation Requirements
Record baseline pressure, adjustments, and verification timestamps to create reliable audit trails. Facilities that digitize calibration logs report 32% fewer therapy interruptions compared to those using manual tracking.
Overpressure Protection: Safety Mechanisms and System Design
Role of Built-In Safety Valves in Preventing Overpressure Events
Modern pressure infusion bags feature spring-loaded safety valves that activate within 0.3 seconds when pressures exceed 200–300 mmHg. These mechanisms reduce air embolism risks by 84% in clinical studies. Recent research analyzing dynamic valve response patterns (Schmidt et al. 2024) confirms their effectiveness across varying temperatures and fluid viscosities common in IV therapies.
Evaluating Pressure Bag Systems for Fail-Safe Features and Usability
Top-tier infusion systems integrate redundant safety valves with visual pressure indicators, achieving 99.6% compliance with IEC 60601-2-24 standards. Key evaluation metrics include:
- Valve reset accuracy (±5 mmHg tolerance)
- Emergency pressure dump speed (<1 second response)
- False positive rate (<0.2% in 10,000-cycle testing)
Dual-stage pressure relief designs demonstrate 40% fewer calibration errors than single-valve models in critical care environments.
Balancing High Flow Demands with Patient Safety: An Industry Challenge
When dealing with trauma resuscitation situations, medical teams need fluid flow rates reaching as high as 1,000 mL per minute. However, they have to keep the pressure below 300 mmHg to prevent damage to blood vessels. That's actually quite a jump from regular procedures, about 72% higher than what's typically required. Engineers working on these systems face some serious design hurdles because of this balance between speed and safety. Some new devices are coming along though that incorporate intelligent pressure regulation technology. These prototypes manage to keep flow variations under 2%, which is impressive considering how critical timing is during emergencies. Most importantly, testing shows they meet all necessary safety standards in nearly every scenario tested so far.
Monitoring Pressure Stability and Managing Re-Inflation Needs
Causes of Pressure Decline: Air Leakage and Fluid Resistance
Keeping therapeutic pressure stable demands close attention to detail. According to a study published in Biomedical Instrumentation Review last year, around one third of all pressure drops happen because air slips through faulty seals or connections. Another problem comes from thick medications that clog narrow IV lines, sometimes causing a 25 mmHg drop each hour. Before starting any procedure, technicians need to check those rubber gaskets and flexible tubes really carefully. Look for cracks, wear spots, or anything that might let air escape over time. These small details matter a lot when trying to maintain proper pressure levels during treatment.
Recommended Intervals for Pressure Checks and Re-Inflation
Clinical protocols recommend checking pressure every 15–30 minutes during infusion. For high-flow applications like contrast delivery, re-inflation to the 200–300 mmHg range may be necessary hourly. Standardizing documentation—including baseline pressures, adjustments, and timestamps—supports both audit readiness and therapy optimization.
Minimizing Flow Rate Variability to Ensure Therapy Consistency
Maintaining ±10% pressure stability reduces flow rate variability by 18% compared to unmonitored systems. Tools such as dual-channel pressure gauges and automated re-inflation alerts help sustain target ranges without disrupting treatment. This level of precision is vital in time-sensitive interventions like thrombolytic administration, where flow inconsistencies exceeding 15% can compromise outcomes.
FAQ
What is the primary purpose of pressure infusion bags?
Pressure infusion bags are used to rapidly deliver fluids to patients by applying additional pressure to standard IV bags, which speeds up the fluid infusion process.
What are the risks associated with pressure infusion bags?
Two major risks include air embolism caused by residual air in the system, and tissue extravasation resulting from excessive pressure which can rupture veins.
How does flow rate variability affect patient therapy?
Inconsistent flow rates can impact emergency treatment protocols needing specific fluid amounts per minute due to loss of fluid pressure over time.
What standards ensure the safety of pressure infusion systems?
Pressure infusion bags must meet ISO 60601-2-34 standards, requiring precise calibration for safe therapeutic flow rates and patient protection.
What are common causes of pressure decline during infusion?
Pressure declines often result from air leakages through faulty seals or connections and fluid resistance from thick medications clogging IV lines.
Table of Contents
- Understanding Pressure Infusion Bags and Associated Clinical Risks
- The Science of Pressure Calibration in Infusion Systems
- Step-by-Step Calibration Best Practices for Pressure Infusion Bags
- Pre-Use Inspection and Initial Inflation Techniques
- Applying Standardized Calibration Procedures for Consistent Pressure Delivery
- Using Pressure Gauges to Achieve and Verify 200–300 mmHg Target Range
- Documenting Calibration Settings and Re-Inflation Requirements
- Overpressure Protection: Safety Mechanisms and System Design
- Monitoring Pressure Stability and Managing Re-Inflation Needs
- FAQ


